Abstract
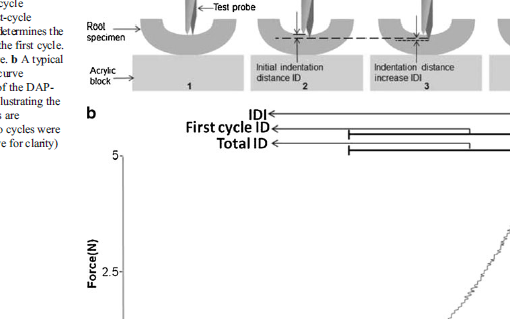
Atypical femoral fractures (AFF) associated with long-term bisphosphonates (LTB) are a growing concern. Their etiology is unknown, but bone material properties might be deteriorated. In an AFF series, we analyzed the bone material properties by microindentation. Four groups of patients were included: 6 AFF, 38 typical osteoporotic fractures, 6 LTB, and 20 controls without fracture. Neither typical osteoporotic fractures nor controls have received any antiosteoporotic medication. A general laboratory workup, bone densitometry by dual-energy X-ray absorptiometry (DXA), and microindentation testing at the tibia were done in all patients. Total indentation distance (Total ID), indentation distance increase (IDI), and creep indentation distance (Creep ID) were measured (microns). Age-adjusted analysis of covariance (ANCOVA) was used for comparisons. Controls were significantly younger than fracture groups. Bisphosphonate exposure was on average 5.5 years (range 5 to 12 years) for the AFF and 5.4 years (range 5 to 8 years) for the LTB groups. Total ID (microns) showed better material properties (lower Total ID) for controls 36 (± 6; mean ± SD) than for AFF 46 (± 4) and for typical femoral fractures 47 (± 13), respectively. Patients on LTB showed values between controls and fractures, 38 (± 4), although not significantly different from any of the other three groups. IDI values showed a similar pattern 13 (± 2), 16 (± 6), 19 (± 3), and 18 (± 5). After adjusting by age, significant differences were seen between controls and typical (p < 0.001) and atypical fractures (p = 0.03) for Total ID and for IDI (p < 0.001 and p < 0.05, respectively). There were no differences in Creep ID between groups. Our data suggest that patients with AFF have a deep deterioration in bone material properties at a tissue level similar to that for the osteoporotic fracture group. The LTB group shows levels that are in between controls and both type of fractures, although not statistically different. These results suggest that bisphosphonate therapy probably does not put the majority of patients at risk for AFF.
https://www.ncbi.nlm.nih.gov/pubmed/22887720
J Bone Miner Res. 2013 Jan;28(1):162-8. doi: 10.1002/jbmr.1731.