Abstract
CONTEXT:
Bone mineral density (BMD) does not fully capture fracture risk as the majority of fractures occur in patients with osteopenia, suggesting that altered bone material properties and changes in microarchitecture may contribute to fracture risk.
OBJECTIVE:
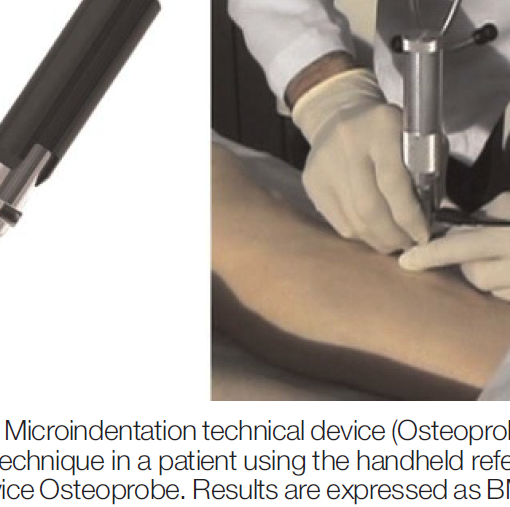
This study aimed to evaluate the relationship between bone material strength (BMS), measured by microindentation in vivo, and fracture in patients with low bone mass.
METHODS:
BMS was measured in 90 patients (mean age, 61.0 y; range, 40.4-85.5 y) with low bone mass with or without a fragility fracture. Sixty-three patients had sustained one or more fragility fractures.
RESULTS:
There was a significant negative correlation between age and BMS (r = -0.539; P < .001) and with the 10-year fracture probability with and without inclusion of femoral neck BMD as calculated by FRAX (r = -0.383; P < .001 and r = -0.426; P < .001, respectively). BMS values were lower in patients with a fragility fracture compared with nonfracture patients (79.9 ± 0.6 vs 82.4 ± 1.0; P = .032) despite similar BMD. BMS was comparable in patients with a fragility fracture whether they had osteopenia or osteoporosis (79.8 ± 0.8 vs 78.7 ± 1.1; P = .456). In patients with osteopenia, BMS was significantly lower in fracture patients than in nonfracture patients (80.3 ± 0.7 vs 83.9 ± 1.2; P = .015).
CONCLUSION:
These data suggest that patients with fractures have altered material properties of bone that are not captured by BMD. Additional studies are required to establish the value of BMS in the prediction of fracture risk, especially in patients with osteopenia.
https://www.ncbi.nlm.nih.gov/pubmed/25768670
J Clin Endocrinol Metab. 2015 May;100(5):2039-45. doi: 10.1210/jc.2014-4346. Epub 2015 Mar 13.