Abstract
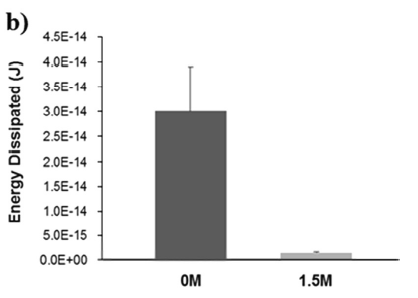
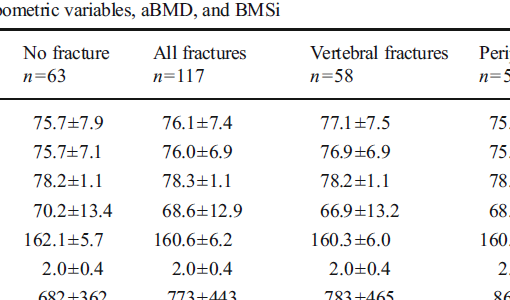
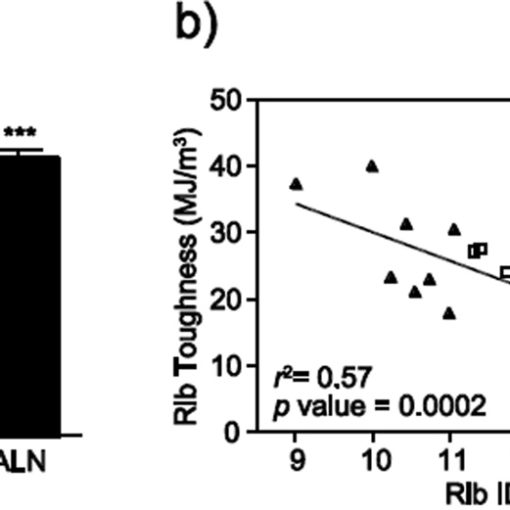
The assessment of fracture risk often relies primarily on measuring bone mineral density, thereby accounting for only a single pathology: the loss of bone mass. However, bone’s ability to resist fracture is a result of its biphasic composition and hierarchical structure that imbue it with high strength and toughness. Reference point indentation (RPI) testing is designed to directly probe bone mechanical behavior at the microscale in situ, although it remains unclear which aspects of bone composition and structure influence the results at this scale. Therefore, our goal in this study was to investigate factors that contribute to bone mechanical behavior measured by cyclic reference point indentation, impact reference point indentation, and three-point bending. Twenty-eight female cadavers (ages 57-97) were subjected to cyclic and impact RPI in parallel at the unmodified tibia mid-diaphysis. After RPI, the middiaphyseal tibiae were removed, scanned using micro-CT to obtain cortical porosity (Ct.Po.) and tissue mineral density (TMD), then tested using three-point bending, and lastly assayed for the accumulation of advanced glycation end-products (AGEs). Both the indentation distance increase from cyclic RPI (IDI) and bone material strength index from impact RPI (BMSi) were significantly correlated with TMD (r=-0.390, p=0.006; r=0.430, p=0.002; respectively). Accumulation of AGEs was significantly correlated with IDI (r=0.281, p=0.046), creep indentation distance (CID, r=0.396, p=0.004), and BMSi (r=-0.613, p<0.001). There were no significant relationships between tissue TMD or AGEs accumulation with the quasi-static material properties. Toughness decreased with increasing tissue Ct.Po. (r=-0.621, p<0.001). Other three-point bending measures also correlated with tissue Ct.Po. including the bending modulus (r=-0.50, p<0.001) and ultimate stress (r=-0.56, p<0.001). The effects of Ct.Po. on indentation were less pronounced with IDI (r=0.290, p=0.043) and BMSi (r=-0.299, p=0.037) correlated modestly with tissue Ct.Po. These results suggest that RPI may be sensitive to bone quality changes relating to collagen.
https://www.ncbi.nlm.nih.gov/pubmed/27021150
Bone. 2016 Jun;87:37-43. doi: 10.1016/j.bone.2016.03.013. Epub 2016 Mar 26.