Abstract
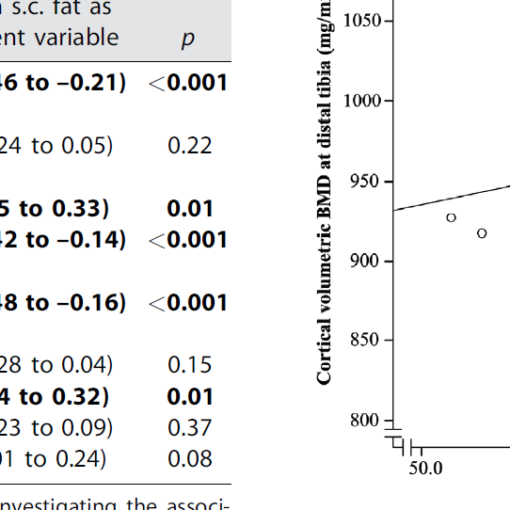
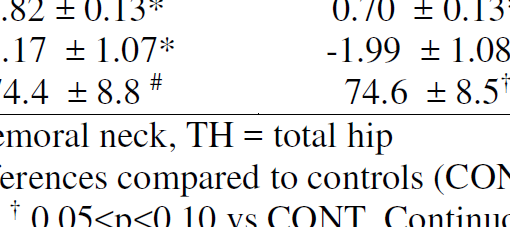
Increased fracture risk, traditionally associated with type 1 diabetes, has lately been of great concern in patients with type 2 diabetes. A variable increase in fracture risk has been reported, ranging from 20% to 3-fold, depending on skeletal site, diabetes duration and study design. Longer disease duration, the presence of diabetic complications, inadequate glycemic control, insulin use and increased risk for falls are all reported to increase fracture risk. Patients with type 2 diabetes display a unique skeletal phenotype with either normal or more frequently increased, bone mineral density and impaired structural and geometric properties. Recently, alterations in bone material properties seem to be the predominant defect leading to increased bone fragility. Accumulation of advanced glycation end-products and changes in collagen cross-linking along with suppression of bone turnover seem to be significant factors impairing bone strength. FRAX score has been reported to underestimate fracture risk and lumbar spine BMD is inadequate in predicting vertebral fractures. Anti-diabetic medications, apart from thiazolidinediones, appear to be safe for the skeleton, although more data are needed. Optimal strategies to reduce skeletal fragility in type 2 diabetic patients are yet to be determined.
https://www.ncbi.nlm.nih.gov/pubmed/25284729
Metabolism. 2014 Dec;63(12):1480-90. doi: 10.1016/j.metabol.2014.09.002. Epub 2014 Sep 28.